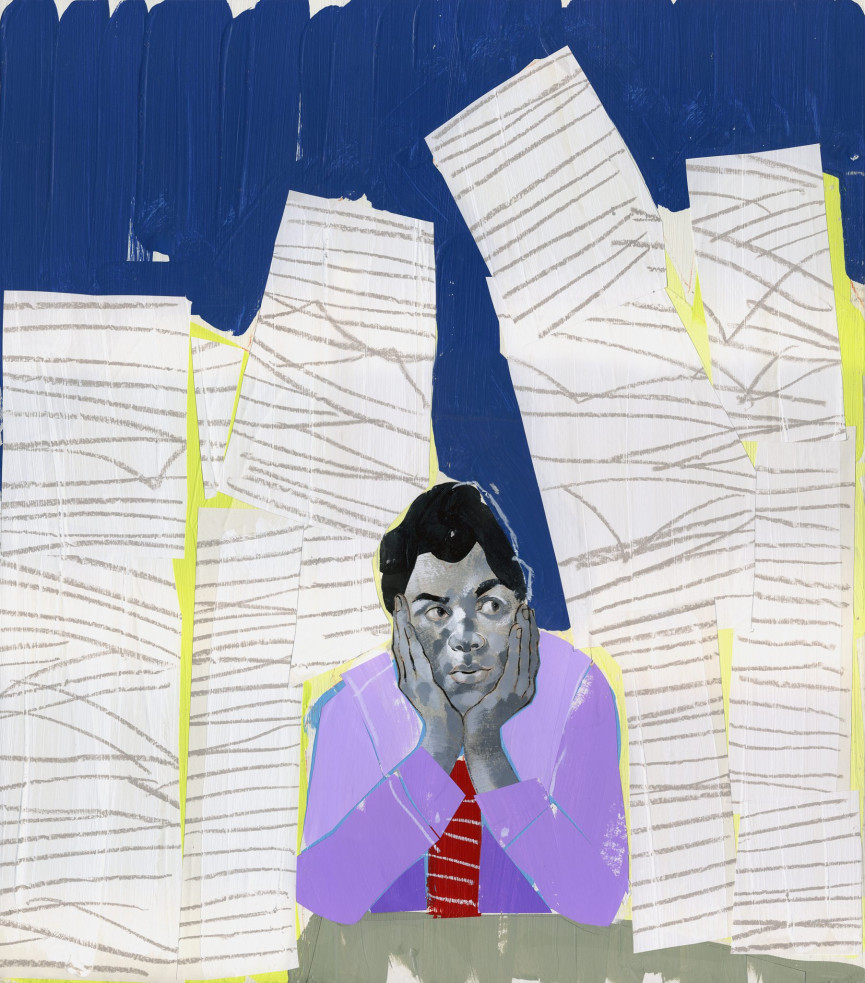
What it feels like to hide your mental health problems from your boss
"I disappear for fifteen minutes every now and again to go break down in my car, or in the toilets"

Picture a man in his late twenties. He’s just had two back-to-back meetings with clients discussing multi-million pound advertising budgets and it’s not eleven o’clock.
He was on the road at half-six this morning for the two hour drive to the office. People call him confident, cocky even. His team love him and he loves them.
At about eleven he gets up and leaves his desk. Outside there are clouds in a northern sky. He gets to his car.
He’s at the height of his career, each new job a promotion with more money. He’s got a girlfriend he really loves. A house. He puts some music on. And he cries. He cries for five, ten minutes, then he’s done.
“It’s simple as that,” says Mark (not his real name). “Probably not the greatest story in the world ‘man suffers from depression so he cries’. It’s just something I do.”
Mark describes his depression as like carrying a backpack “that you keep putting your anxiousness in” but then “you’ll get half way through the day and that backpack’s full and you can’t carry it anymore.”
Walking back to the office, Mark puts his “work face” on and he’s back: the confident, decisive professional that everyone expects. “Right,” he says, “I’ve got to be sarcastic, I’ve got to be funny, I’ve got to be charismatic. That’s the person I made people believe I was from day one.”
Get exclusive shortlists, celebrity interviews and the best deals on the products you care about, straight to your inbox.
Get our best stories, delivered daily for free
Get exclusive shortlists, celebrity interviews and the best deals on the products you care about, straight to your inbox.
Mark was diagnosed with depression and anxiety three and half years ago and he’s never told his boss. According to The Mental Health Foundation, nearly 15 per cent of people experience mental health difficulties while at work.
In theory, having difficulties with your mental health at work shouldn’t be a problem. The Equality Act 2010 gives employees the right to challenge discrimination on a range of protected characteristics like gender, age, ethnic heritage and disability. Mental health difficulty counts as a disability if it causes you long-term, day-to-day difficulties doing things that someone without the same difficulties might reasonably expect to be able to do.
Employers have a legal duty to provide aids and to make reasonable adjustment for disabled employees. Reasonable adjustments include more flexible working hours; the opportunity to work remotely if possible; the provision of aids to assist you in doing your work or other mutually agreed support.
A number of current campaigns in England are trying to help workplaces become more supportive places to be. Some larger employers even provide confidential services known as employee assistance programmes, where staff can contact an outside agency for counselling or other support.
But in practice, being open about your mental health at work is not as simple.
Article continues…
(function(d,s,id){var js,fjs=d.getElementsByTagName(s)[0];if(d.getElementById(id))return;js=d.createElement(s);js.id=id;js.src='https://embed.playbuzz.com/sdk.js';fjs.parentNode.insertBefore(js,fjs);}(document,'script','playbuzz-sdk'));
Esther is in her mid-forties. For most of her adult life she’s experienced mental health difficulties and has survived both abusive relationships and alcohol problems.
A single parent, in 2013 she had the worst year of her life. Her mum got cancer. A close family member revealed a serious alcohol problem. “I felt like my head was going to explode. I was waiting for the breakdown,” she says. Despite this, she was surprised and delighted to land an IT consultancy job.
Almost from the beginning, Esther knew that she wasn’t feeling well. “I was turning up very obviously not OK,” she remembers.
“In the seven weeks I was there I probably did three days worth of work because I spent my time at work worrying about all the things that we’re going on in my life and then I would get home and I would spend the whole of the evening worrying that they were going to find out that I’d done no work that day.”
“I was the breadwinner… I felt like I was giving up, putting my family into poverty”
Esther managed to stick it out for seven weeks before resigning. One of the things that kept her from revealing how much she was struggling was the worry of having her own worst fears about herself confirmed.
“There was a sense of shame and feeling there was something wrong with me. Admitting that there was a problem felt like admitting that I wasn’t up to the task of being a human.
“Shame is just the most toxic thing. If you say ‘I’m struggling’ they might say ‘well, yeah we think you’re crap’.”
Esther worked out she could just about manage on income support. “I was the breadwinner. It didn’t make me feel good, I felt like I was giving up, putting my family into poverty.”
Crashing out of this job gave Esther a chance to get sober and retrain as a yoga teacher. She feels it was the right thing, but it didn’t feel it at the time.
Work is what gives us the money to do things like pay for a place to live; to look after ourselves and our families; and to enjoy our lives. Given the increasingly punitive benefits system, which has been found to discriminate against those with mental health difficulties, the world outside of work looks increasingly difficult.
Elsie (not her real name) is a HR profession in her early thirties who has previously been open with her employers about her bipolar II disorder. She has recently moved outside of the EU to work in a place that doesn’t offer the same legal protections as the UK.
“I found being open about my health to be empowering and enabled me to take control of the situation,” she says of her past jobs. “Feeling like I can’t be open [now] has the opposite effect and I feel like other people have the power over me.” She worries about being caught out.
“I have to be careful what I say about my past”
“I have to be careful what I say about my past. I know I am going to have to rely on myself more and my experience to manage my condition and stay well. I’ve been stable for a long time, but not having someone who can watch and warn me if something seems amiss feels more precarious.”
Elsie believes being open “in a place where there is no data protection, poor record keeping and a bad attitude to mental health” seems “very risky indeed”, but she also worries that she can’t take responsibility for her health at work in the way she has in the past.
“Flexible working helped me manage my health. Here I work a rigid pattern and can’t work from home, so if I’m having a bad day I can’t hide away from people.”
To be open, Elsie would need to feel able to trust that her manager would be non-judgmental and would listen, keep things confidential afterwards, and that it wouldn’t have a negative impact on the way he managed her and treated her at work.
“I know in the UK I am protected,” she says. “Despite being well and stable it would be hard to argue I’m not disabled.” In her current home, there is no legal protection “if things go horribly wrong.”
“I disappear for fifteen minutes every now and again to go break down in my car, or break down in the toilets”
For Mark, putting on his confident work persona doesn’t feel like hiding in the same way. He doesn’t want to make a big thing about his mental health at work.
“In a weird messed up way the most comfortable I am is in work,” he says. “Outside of work I don’t trust people. I don’t want to be around people. I don’t want to go home and make my girlfriend feel unhappy and fill her evening with dread and negativity.
“I’ll pull up in a service station and spend three hours reading stupid websites on my phone. I’ve got it sorted in work. I’ve got it nailed. Yeah, I disappear for fifteen minutes every now and again to go break down in my car, or break down in the toilets. But when I come home I have nothing sorted.”
Surviving work and living up to the persona he’s created while trying to manage his depression and anxiety takes it out of him. “Maybe it’s my own fault for giving this cocky arrogant funny persona. Like nothing really matters to me,” he says.
“The problem for me isn’t ‘can you go into work and host meetings and talk about multi-million pound contracts? The answer is always yes. The other side is ‘can you go home at night and function like a normal person? Can you go home at night and not zone out?’ I’m ashamed that I’m in a relationship where my girlfriend has to do everything.”
Almost as an afterthought, Mark tells me he had handed in his notice. Instead of spending four hours a day driving to and from work, he’s going to have more time to himself, more time with his girlfriend, by working in the town he lives in. For the first time in years he’s going to be able to get more than four or five hours sleep a night. He hopes it will make a difference.
“The team I work for were supportive, they did care, they helped me”
Mark, Elsie, and Esther’s experiences shouldn’t put you off speaking with your boss or seeking the help you need. Miranda is a depression sufferer who lost her career in microbiology after becoming visually impaired two years ago, aged 24. After six months signed off sick, she was redeployed into an admin role.
“I had to learn how to use assistive technology, be mobility trained with a cane and adapt to new surroundings. My confidence plummeted when people would get frustrated with me,” she says.
“I was suffering, constantly on edge. I wasn’t sleeping, I was crying over the littlest thing. The panic attacks were suffocating but I had to keep a smile on my face and remain professional despite my workload piling up.”
One day someone came into Miranda’s office who reminded her of an attacker for a horrible assault she suffered years ago.
“Going to work after this was horrible, I would shake, vomit, make excuses to go home, call in sick.” When Miranda eventually had a meeting with her manager, she was pleasantly surprised by his reaction.
“I broke down after trying to brave it,” she says, explaining she is currently signed off sick.
“Once it all came out it was a relief like a weight lifted but it also showed me that the team I work for were supportive, they did care, they helped me and have stayed in touch to see if I’m OK. This helped a lot.” At present, Miranda is unsure when she will return to work.
“I would shake, vomit, make excuses to go home, call in sick”
Everyone I spoke to in this article sounded vulnerable in different ways. Living with things that happen in your head that other people don’t experience is hard. As the world of work demands more and more from each of us, those of us who face difficulties that others do not will feel the pressure first. According to analysis carried out by The Trades Union Congress in 2017, only 45.5 per cent of people with depression and anxiety were in work. For people with other long term mental health difficulties the total was even lower at 26.2 per cent.
Often, especially at work, it’s when someone most needs the support of others that they most feel the need to hide. We all like to think we can tough things out. When you are feeling at your lowest, it can be hard to trust that your employer will understand and even harder to have faith they will put your interests at an equal footing with those of the organisation. Yet the people I spoke to show silence isn’t always the answer either. If you are suffering, speak with your GP – even if you aren’t quite ready to speak to your boss.
If you have been affected by any of the issues raised in this article please visit mind.org.uk and read their guide to taking care of yourself at work.
(function(d,s,id){var js,fjs=d.getElementsByTagName(s)[0];if(d.getElementById(id))return;js=d.createElement(s);js.id=id;js.src='https://embed.playbuzz.com/sdk.js';fjs.parentNode.insertBefore(js,fjs);}(document,'script','playbuzz-sdk'));
(Pics: Getty)